Flail chest is a life-threatening traumatic injury that occurs when 3 or more contiguous ribs Ribs A set of twelve curved bones which connect to the vertebral column posteriorly, and terminate anteriorly as costal cartilage. Together, they form a protective cage around the internal thoracic organs. Chest Wall: Anatomy are fractured in 2 or more different locations. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship present with chest pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways, tachypnea Tachypnea Increased respiratory rate. Pulmonary Examination, hypoxia Hypoxia Sub-optimal oxygen levels in the ambient air of living organisms. Ischemic Cell Damage, and paradoxical chest wall Chest wall The chest wall consists of skin, fat, muscles, bones, and cartilage. The bony structure of the chest wall is composed of the ribs, sternum, and thoracic vertebrae. The chest wall serves as armor for the vital intrathoracic organs and provides the stability necessary for the movement of the shoulders and arms. Chest Wall: Anatomy movement. Management includes oxygen supplementation, pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways control, ventilation Ventilation The total volume of gas inspired or expired per unit of time, usually measured in liters per minute. Ventilation: Mechanics of Breathing if respiratory failure Respiratory failure Respiratory failure is a syndrome that develops when the respiratory system is unable to maintain oxygenation and/or ventilation. Respiratory failure may be acute or chronic and is classified as hypoxemic, hypercapnic, or a combination of the two. Respiratory Failure presents, and possible surgery. Severe traumatic intrathoracic injuries, such as pulmonary contusions, pneumothorax Pneumothorax A pneumothorax is a life-threatening condition in which air collects in the pleural space, causing partial or full collapse of the lung. A pneumothorax can be traumatic or spontaneous. Patients present with a sudden onset of sharp chest pain, dyspnea, and diminished breath sounds on exam. Pneumothorax, and cardiac injuries, are often seen in conjunction with flail chest.
Last updated: Apr 13, 2025
Flail chest is defined as 3 or more contiguous ribs Ribs A set of twelve curved bones which connect to the vertebral column posteriorly, and terminate anteriorly as costal cartilage. Together, they form a protective cage around the internal thoracic organs. Chest Wall: Anatomy that are fractured in 2 or more different locations, resulting in a freely moving segment of the chest wall Chest wall The chest wall consists of skin, fat, muscles, bones, and cartilage. The bony structure of the chest wall is composed of the ribs, sternum, and thoracic vertebrae. The chest wall serves as armor for the vital intrathoracic organs and provides the stability necessary for the movement of the shoulders and arms. Chest Wall: Anatomy that is discontinuous from the rest of the thoracic cage.
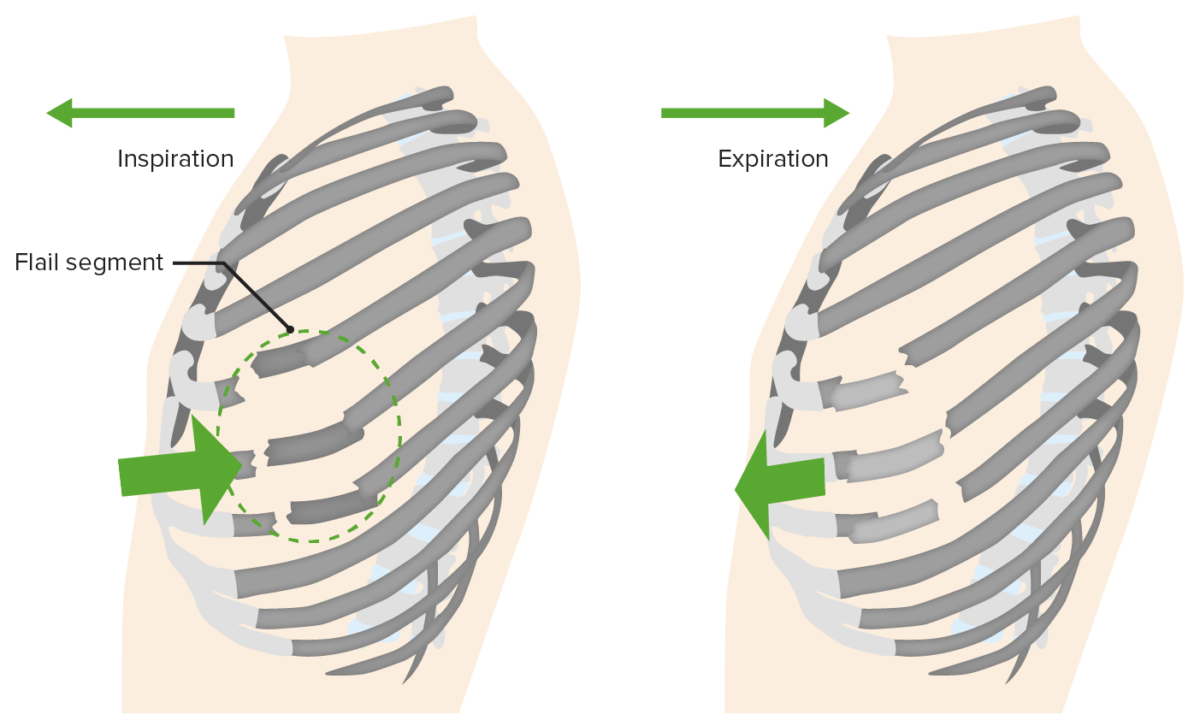
Flail chest
Multiple rib fractures and disruption of structural components of the chest wall (i.e., bone, cartilage, muscle) leading to a free-floating segment of the chest. The separated segment moves opposite to the rest of the chest wall during the breath cycle (paradoxical movement), creating ineffective ventilation.
Flail chest is a clinical diagnosis (confirmed by imaging) made by identifying the paradoxical movement of a chest wall Chest wall The chest wall consists of skin, fat, muscles, bones, and cartilage. The bony structure of the chest wall is composed of the ribs, sternum, and thoracic vertebrae. The chest wall serves as armor for the vital intrathoracic organs and provides the stability necessary for the movement of the shoulders and arms. Chest Wall: Anatomy segment when the patient is spontaneously breathing.
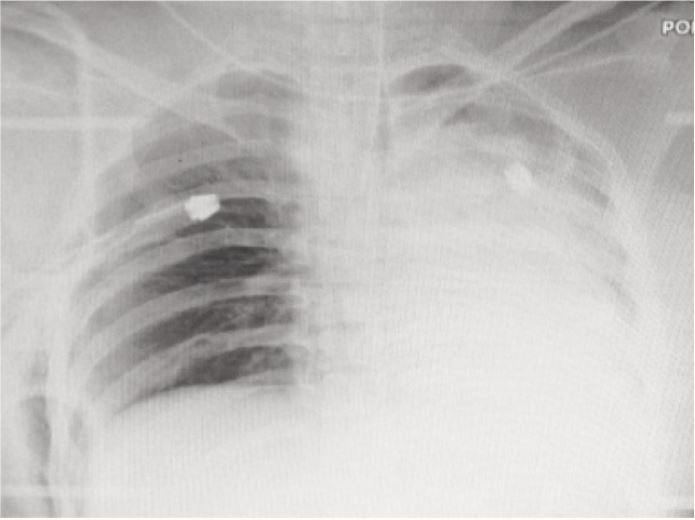
Chest radiograph with rib fractures and pneumothorax
Image: “The Flail and Pulseless Upper Limb: an Extreme Case of Traumatic Scapulo-thoracic Dissociation” by Malaysian Orthopaedic Journal. License: CC BY 3.0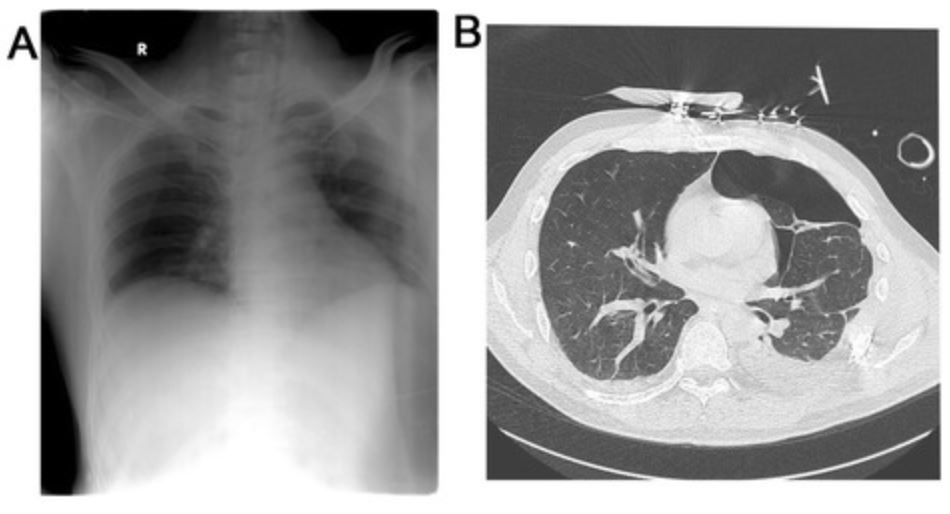
A 55-year-old patient with anterolateral flail chest due to segmental fracture of ribs 4–9 with a hemopneumothorax
A: chest X-ray; B: computed tomography (CT) scan
Pneumothorax Pneumothorax A pneumothorax is a life-threatening condition in which air collects in the pleural space, causing partial or full collapse of the lung. A pneumothorax can be traumatic or spontaneous. Patients present with a sudden onset of sharp chest pain, dyspnea, and diminished breath sounds on exam. Pneumothorax:
Tension pneumothorax Tension Pneumothorax Pneumothorax:
Hemothorax Hemothorax A hemothorax is a collection of blood in the pleural cavity. Hemothorax most commonly occurs due to damage to the intercostal arteries or from a lung laceration following chest trauma. Hemothorax can also occur as a complication of disease, or hemothorax may be spontaneous or iatrogenic. Hemothorax:
Pulmonary contusion:
Acute respiratory distress syndrome Acute Respiratory Distress Syndrome Acute respiratory distress syndrome is characterized by the sudden onset of hypoxemia and bilateral pulmonary edema without cardiac failure. Sepsis is the most common cause of ARDS. The underlying mechanism and histologic correlate is diffuse alveolar damage (DAD). Acute Respiratory Distress Syndrome (ARDS) (ARDS):
Pneumonia Pneumonia Pneumonia or pulmonary inflammation is an acute or chronic inflammation of lung tissue. Causes include infection with bacteria, viruses, or fungi. In more rare cases, pneumonia can also be caused through toxic triggers through inhalation of toxic substances, immunological processes, or in the course of radiotherapy. Pneumonia:
Blunt cardiac contusion: