Advertisement
Advertisement
Advertisement
Advertisement
Vertigo is defined as the perceived sensation of rotational motion while remaining still. A very common complaint in primary care and the ER, vertigo is more frequently experienced by women and its prevalence Prevalence The total number of cases of a given disease in a specified population at a designated time. It is differentiated from incidence, which refers to the number of new cases in the population at a given time. Measures of Disease Frequency increases with age. Vertigo is classified into peripheral or central based on its etiology. Vertigo is a clinical diagnosis, differentiated through history and physical examination findings, most notably nystagmus Nystagmus Involuntary movements of the eye that are divided into two types, jerk and pendular. Jerk nystagmus has a slow phase in one direction followed by a corrective fast phase in the opposite direction, and is usually caused by central or peripheral vestibular dysfunction. Pendular nystagmus features oscillations that are of equal velocity in both directions and this condition is often associated with visual loss early in life. Albinism. Further testing may be required in malignant cases. Management depends on the etiology but certain maneuvers such as the Epley maneuver can be diagnostic and therapeutic.
Last updated: Jan 13, 2023
Advertisement
Advertisement
Advertisement
Advertisement
Advertisement
Advertisement
Advertisement
Advertisement
Vertigo is a clinical symptom described as the perceived sensation of rotational motion while remaining still.
Peripheral:
Central:
Both: multiple sclerosis Sclerosis A pathological process consisting of hardening or fibrosis of an anatomical structure, often a vessel or a nerve. Wilms Tumor
To understand the causes of vertigo, it is important to understand how the human body perceives and maintains balance.
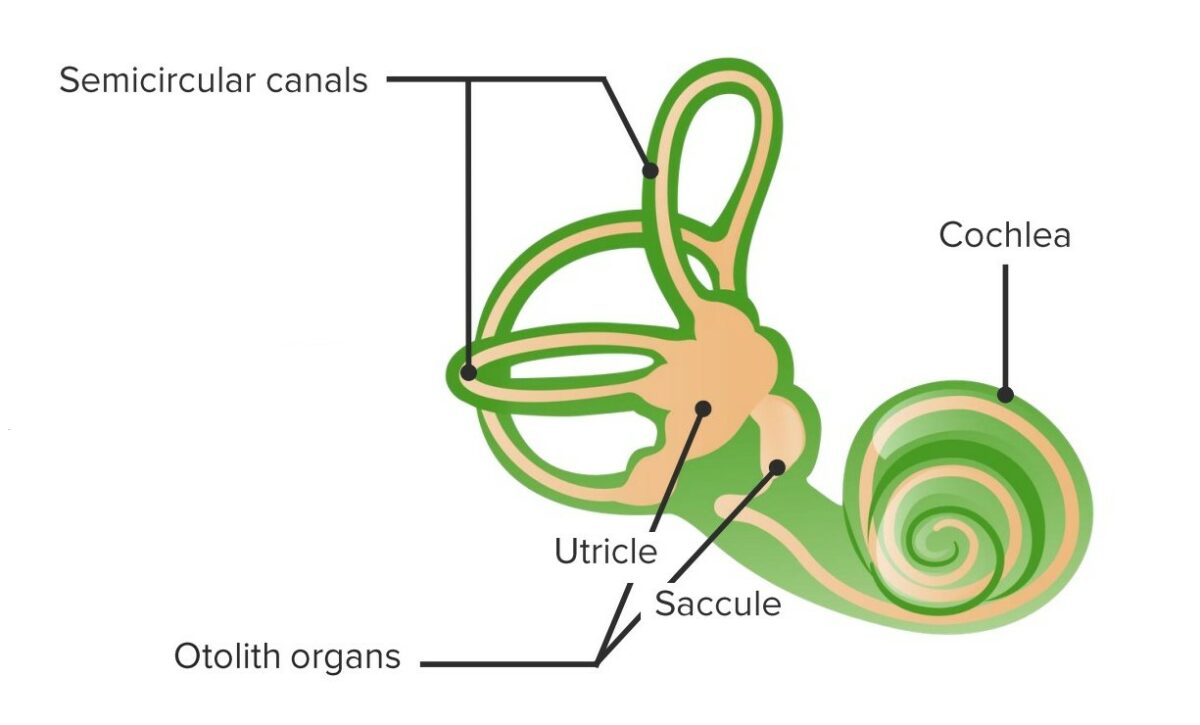
Vestibular structure and function:
The vestibular system is filled with endolymph and communicates with the scala media.
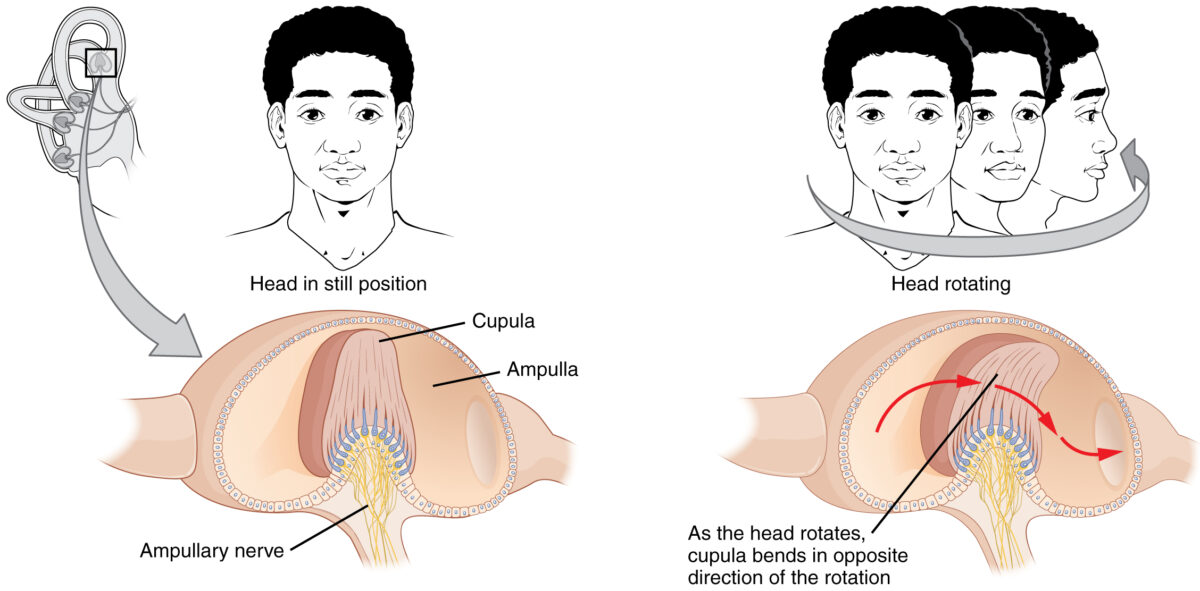
Mechanism of activation of hair cells in the semicircular canals:
When the head is rotated, endolymph courses through the semicircular canals and causes the cupula, which encases the hair cells, to bend in a direction opposite to that of the rotation. When they bend, hair cells depolarize and transmit the signal to the vestibular aspect of cranial nerve VIII.
The chief complaint is dizziness Dizziness An imprecise term which may refer to a sense of spatial disorientation, motion of the environment, or lightheadedness. Lateral Medullary Syndrome (Wallenberg Syndrome).
Vertigo may apparently “decrease” in severity over time, as the affected individual adapts over days to weeks following the onset.
The main goal of physical examination is to differentiate central from peripheral vertigo. If the affected individual additionally complains of hearing loss Hearing loss Hearing loss, also known as hearing impairment, is any degree of impairment in the ability to apprehend sound as determined by audiometry to be below normal hearing thresholds. Clinical presentation may occur at birth or as a gradual loss of hearing with age, including a short-term or sudden loss at any point. Hearing Loss, “Weber” and “Rinne” tests should be performed.
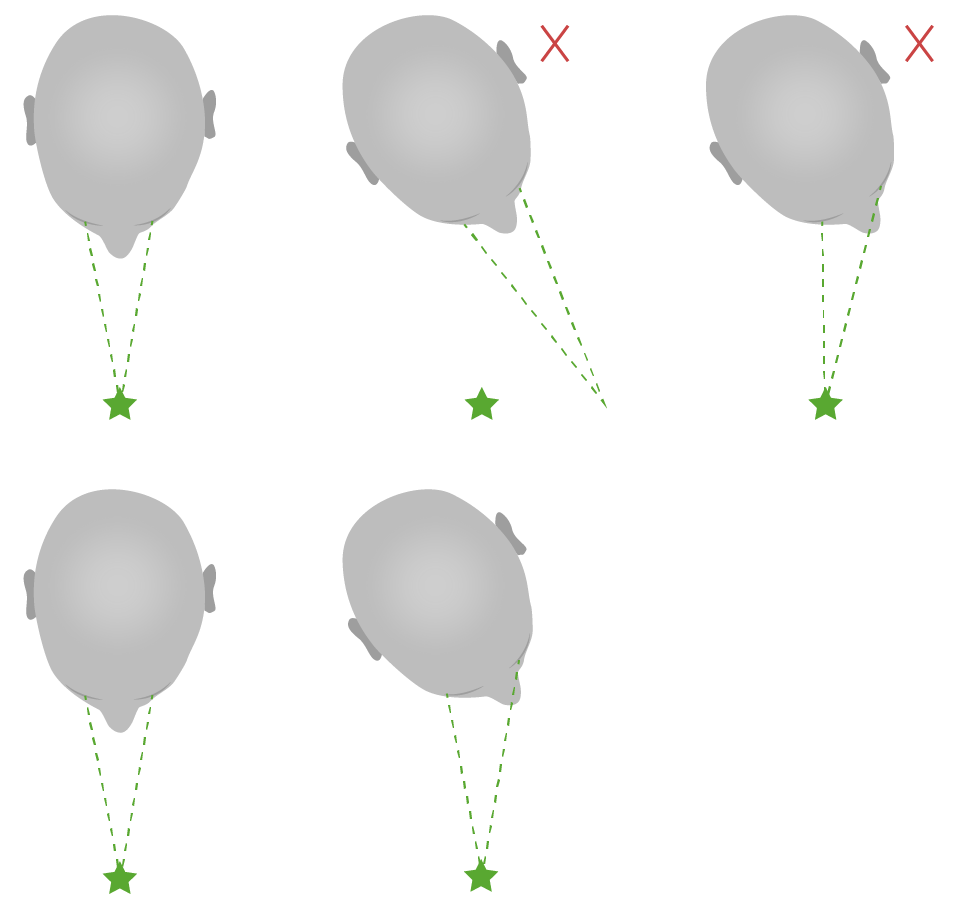
Diagram of abnormal (above) and normal (below) head impulse tests:
Notice that in abnormal situations, the individual’s focal point shifts with the head to later return to the initial point of focus with a saccade.
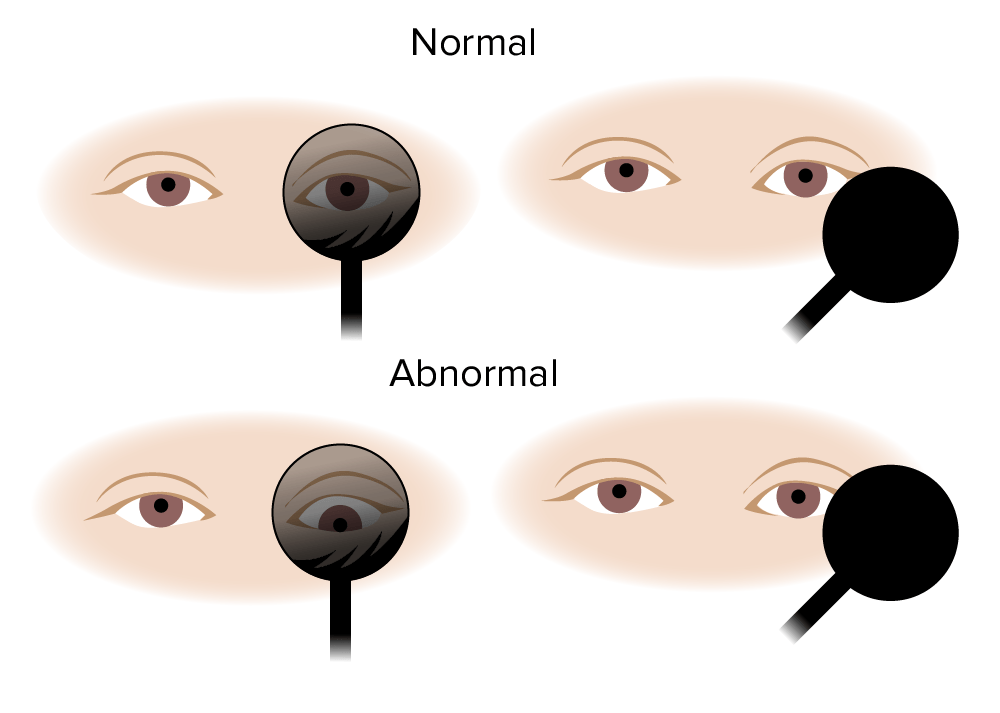
Skew deviation test:
Normally, the eye remains fixed when uncovered. With central lesions, the eye shifts vertically when uncovered.
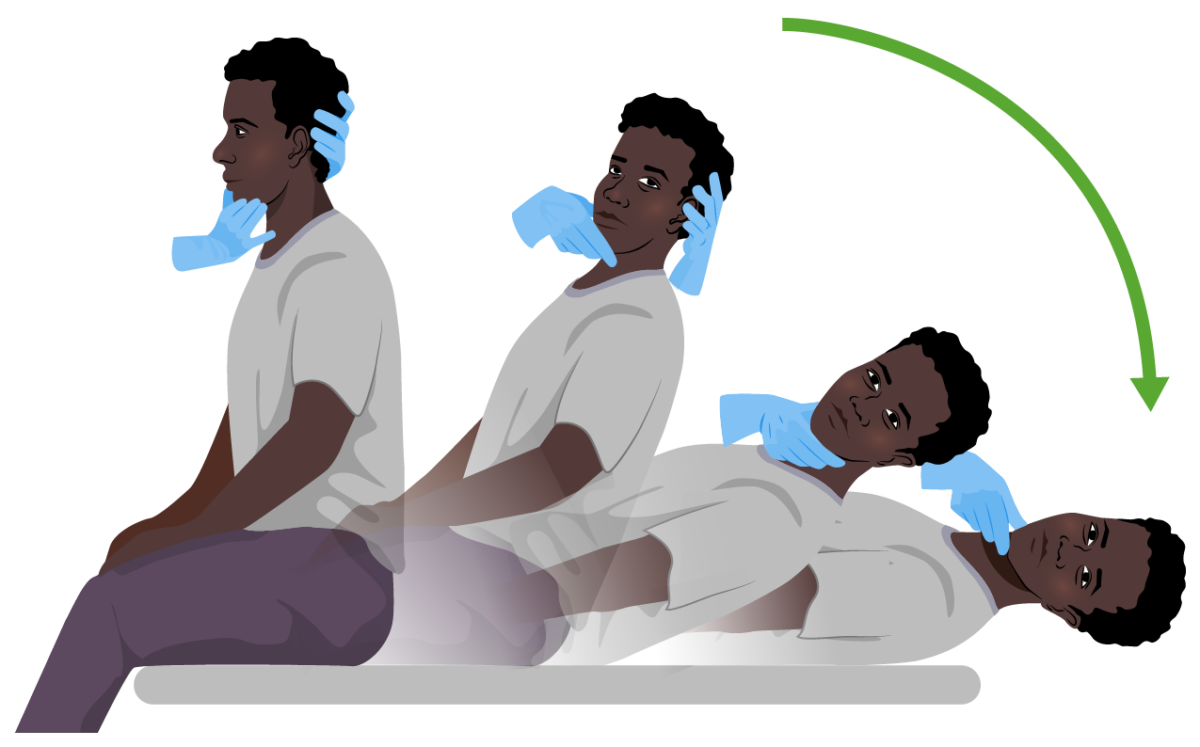
Dix-Hallpike maneuver:
Both diagnostic and curative in benign paroxysmal positional vertigo (BPPV). The subject sits on an examination table and quickly adopts a supine position while the examiner supports their head (to the right or to the left) at a 20º angle below the edge of the bed. The position is held for 30 seconds. In individuals with BPPV, symptoms of vertigo with or without nystagmus become evident.
Vertigo itself is a clinical diagnosis. Further studies are only carried out if more malignant etiologies are suspected.
Definitive management depends on the etiology.
The following conditions can cause dizziness Dizziness An imprecise term which may refer to a sense of spatial disorientation, motion of the environment, or lightheadedness. Lateral Medullary Syndrome (Wallenberg Syndrome) similar to vertigo: